| Abstract |
A 58-year-old male patient presented with pain abdomen since 1 month and bilious vomiting since 1 week. After admission to our hospital, in view of his age and clinical presentation, upper gastrointestinal endoscopy was done and biopsy sent for histopathological examination. A diagnosis of Strongyloidiasis of duodenum was made. Herein, we report such an unusual case, where the diagnosis was first made by duodenal biopsy, rather than simple stool examination. Since the case clinically masqueraded as gastric malignancy, the importance of routine simple stool examination and role of pathologist in identifying the parasite is hereby highlighted.
Keywords: Duodenum, stool examination, Strongyloidiasis
| How to cite this article: Murthy V S, Geethamala K, Kumar B D, Rao M S. Strongyloidiasis of duodenum clinically masquerading as gastric malignancy. Ann Trop Med Public Health 2013;6:248-50 |
| How to cite this URL: Murthy V S, Geethamala K, Kumar B D, Rao M S. Strongyloidiasis of duodenum clinically masquerading as gastric malignancy. Ann Trop Med Public Health [serial online] 2013 [cited 2020 Aug 8];6:248-50. Available from: https://www.atmph.org/text.asp?2013/6/2/248/116494 |
| Introduction |
Strongyloidiasis is a parasitic disease caused by a nematode helminth, Strongyloides stercoralis. The parasite is widely distributed in the soil throughout tropical and subtropical areas, but the true prevalence of S. stercoralis is likely underestimated because infection is often subclinical. [1],[2] Currently an estimated 100 million people are infected worldwide but only few cases have been reported from India, where its prevalence appears to be low. [1],[3] Typically, the infection is asymptomatic and manifests as vague and non-specific gastrointestinal (GI) symptoms. [1] The diagnosis of Strongyloidiasis in humans is based on findings of rhabditoid larvae of S. stercoralis present in the fecal material. The histologic diagnosis of Strongyloidiasis from biopsies and surgical specimens is usually performed incidentally. [4],[5] Herein, we report such an unusual case, where the diagnosis was first made by duodenal biopsy, rather than simple stool examination. Since the case clinically masqueraded as gastric malignancy, the importance of routine simple stool examination and role of pathologist in identifying the parasite is hereby highlighted.
| Case Report |
A 58-year-old male presented with history of pain abdomen of 1 month duration and bilious vomiting since 1 week. His past medical history was of pain abdomen since 1 year for which he was treated symptomatically. He is a known smoker and alcoholic. On physical examination, the patient was poorly built and nourished, pale and anorexic. No generalized lymphadenopathy or edema. Abdominal examination revealed tenderness in the epigastric region. No mass or hepatosplenomegaly.
Laboratory examination revealed microcytic hypochromic anemia with eosinophilia (Hb 6.8 g%, AEC-700 cells/mm 3 ). Liver and kidney function tests were within normal limits and serological tests for HIV, hepatitis B surface antigen (HBsAG) and Venereal Disease Research Laboratory test (VDRL), HBsAG and VDRL were negative. No abnormality was detected on chest X-ray and ultrasound abdomen. Since the patient was elderly, gastric malignancy was suspected and investigated with upper GI endoscopy which showed normal mucosa of esophagus, gastric and duodenum. Biopsies were taken and sent for histopathological examination.
The formalin fixed, H and E stained sections of duodenal biopsies showed florid S. stercoralis infestation with eggs, both larval and adult forms of the parasite within the crypts of duodenal mucosa and even on the surface epithelium [Figure 1] and [Figure 2]. The lamina propria showed inflammatory infiltrates consisting of neutrophils, eosinophils, few lymphocytes and plasma cells. A histopathological diagnosis of Strongyloidiasis of duodenum was made. Subsequently stool examination was carried out which revealed heavy parasitization by S. stercoralis showing rhabditiform larvae having bulbous enlargement at esophageal end and slender tail end [Figure 3] and [Figure 4]. Patient was put on albendazole 400 mg twice daily for 14 days and recovered completely. On the 15 th day stool examination was done which did not reveal any parasite. His family members were also screened and no parasites were identified in the stool examination.
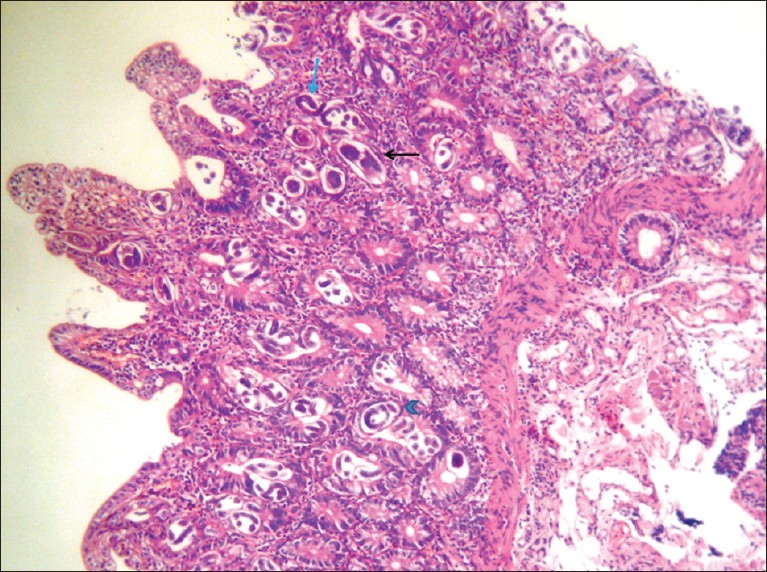 |
Figure 1: Photomicrograph of duodenal mucosa – eggs (black arrow), larval (blue arrow head) and adult forms (blue arrow) of Strongyloides stercoralis within the crypts and surface epithelium (H and E, ×100) |
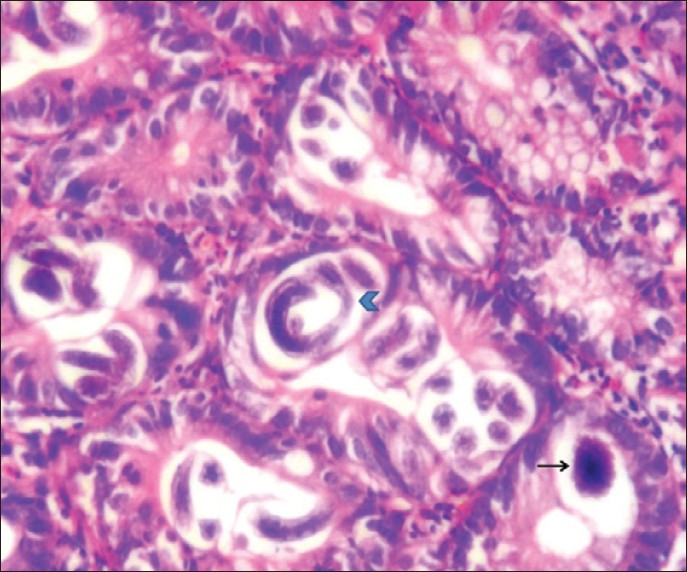 |
Figure 2: Photomicrograph of duodenal mucosa – eggs (black arrow) and larval form (blue arrow head) of Strongyloides stercoralis within the glands (H and E, ×400) |
| Figure 3: Stool smear examination – rhabditiform larvae (Pap, ×100)
Click here to view |
| Figure 4: Stool smear examination – rhabditiform larvae (Pap, ×400)
Click here to view |
| Discussion |
Strongyloidiasis was first described in 1876 in French colonial troops suffering from diarrhea in Vietnam. [1] It is common intestinal infection caused by two species of the nematode Strongyloides. The most common and clinically important pathogenic species in humans is S. Stercoralis. Other species is Strongyloides fuelleborni, which cause limited infections in humans. [1]
The GI manifestations of Strongyloidiasis include abdominal pain, watery diarrhea, constipation, anorexia, weight loss, nausea, and bilious vomiting. [1],[6] These symptoms begin about 2 weeks after infection with larvae which are detectable in stool after 3-4 weeks. [7] Less frequently malabsorption syndrome, paralytic ileus, intestinal obstruction and GI bleeding may occur. The term disseminated disease is used when the infective larvae migrate from the intestine to lungs and to other organs usually not involved in the normal helminthic life cycle. Larva currens is pathognomonic cutaneous manifestation of Strongyloides infection. [1],[3],[8]
The life cycle of this parasite is very complicated. The filariform larvae penetrate the intact skin by contact with infected soil and into the venous microcirculation via lymphatics. Larvae penetrate pulmonary alveoli, ascend the respiratory tree through which they enter pharynx and then are swallowed into stomach and small intestine. In the duodenum larvae mature into adult female. By parthenogenesis female worms produce up to 40 eggs/day. Eggs are 50-58 μ by 30-36 μ in size, delimited by a thin cuticle mostly transparent with either morula or tadpole stages of rhabditoid embryo inside. Once these eggs hatch, rhabditiform larvae are released which can either be passed in stools, continuing their soil based cycle or can cause autoinfection. [1],[8]
The diagnosis of Strongyloidiasis by routine stool examination is very limited, since output of the parasite in the stool is lower and 50-70% of single general stool examination is unrewarding. It is also important to note that the absolute eosinophilic count is not a reliable indicator of parasitic infection. [8] ELISA- Enzyme-linked immunosorbent assay for diagnosing Strongyloidiasis is highly sensitive but the test is not always available, cannot differentiate from recent or old infection and also shows cross reactions with other helminthic infections. [3],[8]
The findings of upper GI endoscopy in Strongyloidiasis have been described as enlarged gastric folds, gastric ulcers, edema and hypertrophy of duodenal mucosa. Small bowel obstruction is secondary to intense infestation. [4],[5],[6] In our case there were no significant findings. Thus, histopathological examination of tissue sections provides definite diagnosis. For the accurate diagnosis, the pathologist needs to have a wide knowledge of the types, their stages of development and morphological features of the helminths to avoid misdiagnosis. [8] In our case, diagnosis was done by histopathological examination alone, of the biopsy specimen.
Characteristic biopsy features of duodenitis are villous atrophy, ulceration, crypt distortion, infiltration of the lamina propria with plasma cells and eosinophils. Strongyloides eggs, larvae and adult worms seen both within the crypts and surface epithelium. [7],[8],[9] The degree of reactive pathologic changes of the duodenal mucosa, particularly the infiltration by eosinophils in the lamina propria, appeared to be related to the intensity of the infection. [5] Our case also showed similar findings.
The awareness of Strongyloidiasis is low in India and there have been only few case reports which have all termed the condition as rarity. Incidence of Strongyloidiasis has been reported as less than 1% in Indian population with heavy parasitic infestation. [3] In patients receiving long-term corticosteroid therapy, malnutrition and immunocompromised, Strongyloidiasis leads to disseminated or hyperinfection syndrome resulting in mortality rates up to 87%. [9]
| Conclusion |
The present case highlights the importance of basic investigation like stool examination before subjecting the patient to invasive procedure. The role of histopathologists is to arrive at a definite diagnosis of the infection by the examination of gastric or duodenal biopsy so as to start the treatment as soon as possible in order to avoid fatality due to systemic dissemination or hyperinfection.
| References |
| 1. | Cruz RJ Jr, Vincenzi R, Ketzer BM. Duodenal obstruction-an unusual presentation of Strongyloides stercoralis enteritis: A case report. World J Emerg Surg 2010;5:23. |
| 2. | Devi U, Borkakoty B, Mahanta J. Strongyloidiasis in Assam, India: A community based study. Trop Parasitol 2010;1:30-2. |
| 3. | Mani RK, Sardana R, Chawla R, Bansal A, Kanwal MS, Arora DS, et al. Respiratory failure, coma and cutaneous lesions due to disseminated strongyloidiasis. Indian J Crit Care Med 2003;7:132-6. |
| 4. | Mohamed AE, Ghandour ZM, Al-Karawi MA, Yasawy MI, Sammak B. Gastrointestinal parasites presentations and histological diagnosis from endoscopic biopsies and surgical specimens. Saudi Med J 2000;21:629-34. |
| 5. | Rivasi F, Pampiglione S, Boldorini R, Cardinale L. Histopathology of gastric and duodenal Strongyloides stercoralis locations in fifteen immunocompromised subjects. Arch Pathol Lab Med 2006;130:1792-8. |
| 6. | Prakash G, Gupta RK, Prakhya S, Balakrishnan R. Concurrent infection of candidiasis and strongyloidiasis in an endoscopic biopsy in an immunocompetent host. Indian J Pathol Microbiol 2011;54:644-5. |
| 7. | Vithayasai N, Jennuvat S. Gastrointestinal manifestations in severe strongyloidiasis: Report of 3 cases and literature review. Southeast Asian J Trop Med Public Health 2010;41:22-7. |
| 8. | Al-Sajee DM, Al-Hamdani A. A case of gastric and duodenal strongyloidiasis. Sultan Qaboos Univ Med J 2010;10:262-5. |
| 9. | Altintop L, Cakar B, Hokelek M, Bektas A, Yildiz L, Karaoglanoglu M. Strongyloides stercoralis hyperinfection in a patient with rheumatoid arthritis and bronchial asthma: A case report. Ann Clin Microbiol Antimicrob 2010;9:27. |
Source of Support: None, Conflict of Interest: None
| Check |
DOI: 10.4103/1755-6783.116494
| Figures |
[Figure 1], [Figure 2], [Figure 3], [Figure 4]



