How to cite this article:
Kumar K J, Mamatha S, Kudakasseril AS, Manjunath V G. Lung abscess in a child. Ann Trop Med Public Health 2012;5:48-9 |
How to cite this URL:
Kumar K J, Mamatha S, Kudakasseril AS, Manjunath V G. Lung abscess in a child. Ann Trop Med Public Health [serial online] 2012 [cited 2020 Aug 14];5:48-9. Available from: https://www.atmph.org/text.asp?2012/5/1/48/92884 |
Sir,
Pediatric pulmonary abscess is a rare respiratory problem in childhood. The incidence of lung abscess in children is 0.7 per 100,000 admissions per year. [1] Advances in the field of antibiotics have drastically reduced the incidence of lung abscesses that too in children. [2] We are reporting a 18 month-old baby with lung abscess and is probably one of the few cases reported in the literature in the modern antibiotic era.
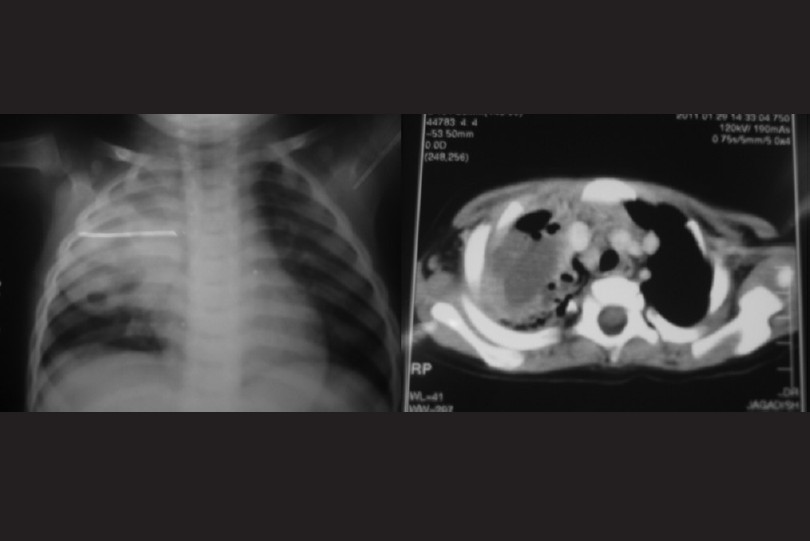
18 month-old baby developmentally normal girl was presented with history of cough, fever, and respiratory distress for the past 7 days. On examination, she was 8 kg, febrile (103°F), and respiratory rate 66/min with respiratory distress. Auscultation revealed bronchial breath sounds in the right mammary, infraaxillary, and right interscapular areas. Rest of the examination was normal. Investigations revealed the following: hemoglobin 8.5 gm/dl, total leucocyte count 17500/mm 3 , platelet count 3.6 lakhs/mm 3 , HIV negative, and kidney function tests were normal. Blood and urine cultures were sterile. The chest radiograph demonstrated a large well-circumscribed consolidated lesion of the right upper lobe with an air fluid level [Figure 1]. Computed tomography scan of the chest confirmed the presence of 45-mm-thick walled cavitatory lesion with air fluid level in the right upper lobe with surrounding normal lung tissues consistent with an abscess [Figure 1]. She was treated with intravenous ceftriaxone, linezolid, and amikacin for 2 weeks followed by oral amoxy clavulanic acid for 3 weeks. She became afebrile within 6 days of antibiotics and remained so for the rest of her hospital stay.
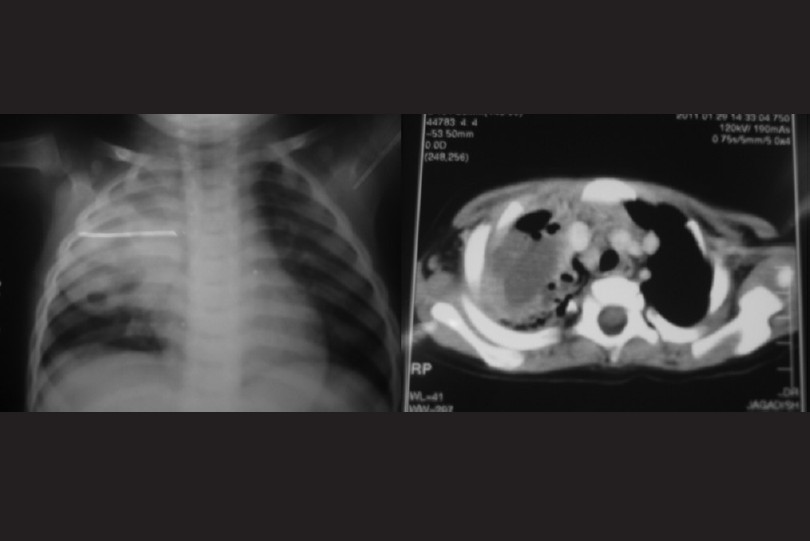 |
Figure 1: The chest radiograph demonstrates a large well-circumscribed consolidated lesion of the right upper lobe with an air fluid level and computed tomography scan of chest showing 45-mm-thick walled cavitatory lesion with air fluid in the right upper lobe
Click here to view |
A lung abscess is a localized infection with central necrosis and suppuration of the lung parenchyma, surrounded by a thick wall of infected and inflammatory tissue. This process may establish communication with an airway and cause partial expectoration of the purulent content and a resultant air-fluid level. Primary lung abscesses are those occurring in otherwise healthy children, whereas secondary are those developing in a child with predisposing factors such as aspiration, pneumonia, cystic fibrosis, gastroesophageal reflux, or immunodeficiency. A primary lung abscess is almost always solitary, whereas secondary abscess can be solitary or multiple. Primary lung abscess occurs predominantly on the right side like in our case and if aspiration is the cause then the upper lobes of either side are commonly involved. Lung abscess in pediatric patients is believed to develop secondary to bacterial pneumonia. [2] The predominant pathogens isolated from primary lung abscesses include streptococcal species, Staphylococcus aureus, and Klebsiella pneumonia. [3] Common differential diagnosis includes infected congenital cystic abnormalities of the lung such as bronchogenic cyst, cystic adenomatoid malformation, and late-presenting congenital right-sided diaphragmatic hernia. [2] Children with a lung abscess, both primary and secondary, have a significantly better prognosis than adults. [3] Lung abscess can be diagnosed by a chest radiographic scan showing a thick-walled cavity containing an air-fluid level. [1] Review of 23 lung abscess children over a 20-year period revealed 11 primary and 12 secondary abscesses, and they could isolate pathogens in 16 patients only, and the most common microorganism was Streptococcus pneumonia. [4] In a retrospective study from Taiwan out of 27 children over a period of 16 years, 70% had underlying chronic diseases, and positive yield rate from aspiration of lung abscess was 63.6%. [5] The treatment of choice for lung abscess is conservative medical management, which should include a parenteral antibiotic with gram-positive activity against both Staphylococcus aureus and anaerobes for a minimum of 3 weeks. [2],[6] Lobectomy should be reserved for those with very severe abscesses and who does not show clinical and radiologic evidence of improvement after at least 3 weeks of appropriate intravenous antibiotic therapy. [6]
| 1. |
Tan TQ, Seilheimer DK. Pediatric lung abscess: Clinical management and outcome. Pediatr Infect Dis J 1995;14:51-5. |
| 2. |
Mishra R, Mishra T, Ratan K, Abrol P, Kadian Y. Right upper lobe lung abscess in an infant. Internet J Surg 2009;20:1. |
| 3. |
Patradoon-Ho P, Fitzgerald DA. Lung abscess in children. Paediatr Respir Rev 2007;8:77-84. |
| 4. |
Yen CC, Tang RB, Chen SJ, Chin TW. Pediatric lung abscess: A retrospective review of 23 cases. J Microbiol Immunol Infect 2004;37:45-9. |
| 5. |
Chan PC, Huang LM, Wu PS, Chang PY, Yang TT, Lu CY, et al. Clinical management and outcome of childhood lung abscess: A 16-year experience. J Microbiol Immunol Infect 2005;38:183-8. |
| 6. |
Emanuel BA, Shulman ST. Lung abscess in infants and children. Clin Pediatr (Phila) 1995;34:2-6. |
Source of Support: None, Conflict of Interest: None
DOI: 10.4103/1755-6783.92884
[Figure 1] |