| Abstract |
We report two cases of bilateral corneal blindness. The first case was a 38-year-old male who presented with bilateral corneal abscesses after a whitish powder was instilled into his eyes by a snake charmer following a snakebite on his right foot. The left eye responded to medical management with intensive topical antibiotics and in the right eye, a penetrating keratoplasty was performed to salvage vision. Another 19-year-old male sustained a similar injury. The right eye responded to medical management and a large-diameter lamellar keratoplasty with symblepharon release was performed for limbal stem cell deficiency in the left eye. Use of traditional eye medicines by snake charmers is still rampant in rural areas of developing countries. Awareness among medical practitioners and the general population is important to avoid the serious blinding consequences of this menace.
Keywords: Corneal blindness, snakebite, traditional medicinal practice
| How to cite this article: Kandar AK, Chawla B, Agarwal P, Tandon R. Corneal blindness following traditional medicinal practices after snakebite. Ann Trop Med Public Health 2010;3:80-2 |
| How to cite this URL: Kandar AK, Chawla B, Agarwal P, Tandon R. Corneal blindness following traditional medicinal practices after snakebite. Ann Trop Med Public Health [serial online] 2010 [cited 2020 Aug 14];3:80-2. Available from: https://www.atmph.org/text.asp?2010/3/2/80/77197 |
| Introduction |
India is a tropical country and a habitat for many varieties of snakes, poisonous as well as non-poisonous. Ocular complications due to snakebite are relatively uncommon. Painful conjunctivitis and lid edema are known to occur when venom is sprayed or ‘spat’ into the eyes by certain cobras in Asia and Africa. [1] Ocular complications described include conjunctival bleeding, uveitis, corneal ulceration and ocular perforation. [2],[3],[4] The eye may also be involved due to the neurological or hematological consequences of snakebite. [5],[6]
Herein, we report two interesting cases of bilateral corneal blindness following the use of traditional eye medicines for treatment of snakebite at a rural setup and their subsequent management at our tertiary care eye hospital following referral.
| Case Reports |
Case 1
A 38-year-old male presented to us 10 days after a snakebite on his right foot. History of presenting illness revealed that during treatment for snakebite at a local village healthcare facility, a traditional eye medicine in the form of a whitish flaky powder was instilled into both his eyes on the advice of a snake charmer. Two days later, the patient developed pain, redness and diminution of vision in both eyes which was diagnosed elsewhere as bilateral corneal ulcers and subsequently referred to our centre for management.
At presentation, ocular examination revealed visual acuity of light perception in both eyes with inaccurate projection. Both the lids were edematous with perilimbal conjunctival congestion. Bilateral corneal abscesses involving the entire cornea were seen, along with corneal perforation and iris pro-lapse OD [Figure 1]a, b. The right cornea had corneal abscess measuring 9.6 × 10.0 mm with a crescentic temporal perforation. The left eye had a corneal abscess measuring 7.4 × 9.0 mm with edema involving the remaining of the cornea. The intraocular pressure was normal to low digitally in both eyes. Posterior segment evaluation on B-scan ultrasonography was unremarkable in both eyes. Systemic examination showed cellulitis of the right foot extending up to the ankle around the area of snakebite. No other systemic abnormality was found.
| Figure 1a: Corneal abscess with perforation in the right eye of Case 1 at presentation Figure 1b: Corneal abscess in the left eye of Case 1 at presentationClick here to view |
A corneal scraping was taken from both eyes and smear preparation showed the presence of Gram-positive cocci. Culture growth was consistent with coagulase-negative Staphylococcus. Blood coagulation profile, renal and liver function tests were normal. Chemical analysis of the powder revealed potassium nitrite. The patient was advised concentrated 5% cefazolin eye drops at hourly intervals, gatifloxacin 0.3% one-hourly and homatropine hydrobromide 2% eye drops four times a day. Systemic cloxacillin 500 mg QID for one week was given for the treatment of foot cellulitis. The right eye continued to worsen and a therapeutic penetrating keratoplasty with lens aspiration was performed two weeks later. The corneal abscess in the left eye responded to medical management with intensive topical antibiotics. Four months later, the graft in the right eye was clear with Best Corrected Visual Acuity (BCVA) of 20/80 [Figure 2]a. The left eye showed an adherent leucoma with a visual acuity of light perception and inaccurate projection [Figure 2]b. Further surgical intervention in the left eye was deferred in view of poor visual prognosis.
| Figure 2a: Clear graft in the right eye of Case 1 after penetrating keratoplasty Figure 2b: Adherent leucoma in the left eye of Case 1 after medical managementClick here to view |
Case 2
A 19-year-old male had a similar history. After snakebite, a powder of unknown nature was instilled into both his eyes by a snake charmer in a village. At the time of presentation, visual acuity was 2/60 OD and light perception with accurate projection OS. Ocular examination of the right eye revealed ischemia involving 120° of the limbus and an epithelial defect 3.5 x 3.2 mm. Examination of the left eye showed a 360° limbal ischemia, an epithelial defect of 7.5 x 8 mm with fibrinous exudates in the anterior chamber. A diagnosis of Grade 2 chemical injury OD and Grade 4 chemical injury OS was made. The intraocular pressure was normal in both eyes. Both the lenses were clear. Posterior segment was unremarkable on ultrasonography in both eyes. The powder was not available for chemical analysis.
The acute stage was managed medically with frequent topical prednisolone acetate 1%, sodium citrate 10%, sodium ascorbate 10%, chloramphenicol 0.3%, cycloplegics and lubricants in both eyes. Amniotic membrane transplantation was performed in the left eye using cryopreserved amniotic membrane. Six months later, visual acuity was 20/30 OD and perception of light with accurate projection OS [Figure 3]a, b. Subsequently, a large-diameter lamellar keratoplasty with symblepharon release was performed for limbal stem cell deficiency in the left eye. Thereafter, the patient was lost to follow-up.
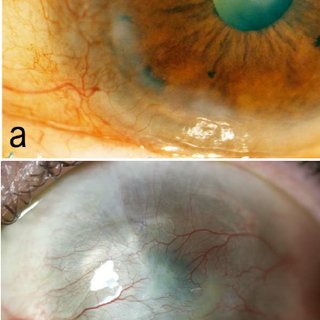 |
Figure 3a: Right eye localized limbal stem cell defi ciency after medical management of Case 2 Figure 3b: Left eye 360° limbal stem cell defi ciency after medical management of Case 2Click here to view |
| Discussion |
Snakebite can produce ocular injuries either directly or indirectly. Chen et al. have reported penetrating injury of the eye leading to severe damage due to direct envenomation. [7],[8],[9] They proposed early evisceration as the treatment of choice for treatment of a penetrating ocular injury caused by venomous snakebite. Unilateral or bilateral vitreous hemorrhage with or without ghost cell glaucoma has also been reported due to viper snakebite. These ocular complications are usually associated with systemic bleeding disorders. [10] The term “snake venom ophthalmia” has been coined to describe the direct and indirect effects of snakebite and subsequent eye injury. [11],[12],[13] Other ocular manifestations, either directly or indirectly after snakebite include extra-ocular muscle palsy which may occur following a cobra bite leading to neuroparalysis. [5]
In our cases the ocular complications were due to neither the direct nor systemic effect of snakebite. Our patients were the victims of illiteracy and myths surrounding snakebites. Use of traditional eye medicines is apparently still rampant in rural areas. Various agents are still being used by snake charmers with serious blinding consequences, especially in rural India. By reporting these cases we would like to make the ophthalmologists and general medical practitioners aware of these possibilities during care of snakebite patients. Also, efforts need to be made to increase public awareness to avoid the serious blinding consequences of this menace.
| References |
| 1. | Gupta M, Sharma P, Jain A, Solanky J, Sharma KK, Basu S. Unusual site of snake bite. Trop Doct 1995;25:134-5. |
| 2. | Price. In Price’s Text book of the Practice of Medicine. Edited by Sir Ronald Bodley Scott ; 10 th edition 1966, Publisher Oxford University Press, London. |
| 3. | Bucaretchi F, Hyslop S, Mello SM, Vieira RJ. Bothrops snakebite on the head: Case report and review of the literature. Ann Trop Med Parasitol 2007;101:733-43. |
| 4. | Warrell DA, Ormerod LD. Snake venom ophthalmia and blindness caused by the spitting cobra (Naja nigricollis) in Nigeria. Am J Trop Med Hyg 1976;25:525-9. |
| 5. | Takeshita T, Yamada K, Hanada M, Oda-Ueda N. Case report: Extraocular muscle paresis caused by snakebite. Kobe J Med Sci 2003;49:11-5. |
| 6. | Ghosh AK, Bhaduri G, Sarkar AD, Mondal LK, Maiti A, Kishore V, et al. Unilateral loss of vision following snakebite. J Indian Med Assoc 2006;104:404-5. |
| 7. | Chen CC, Yang CM, Hu FR, Lee YC. Penetrating ocular injury caused by venomous snakebite. Am J Ophthalmol 2005;140:544-6. |
| 8. | Sheard RM, Smith GT. Penetrating eye injury following a snake attack. Eye 2003;17:279-80. |
| 9. | Korn BS, Korn TS. Cyanoacrylate repair of laser in situ keratomileusis corneal flap perforation by a snake bite. J Cataract Refract Surg 2005;31:2224-6. |
| 10. | Rojas L, Ortiz G, Gutierrez M, Corredor S. Ghost cell glaucoma related to snake poisoning. Arch Ophthalmol 2001;119:1212-3. |
| 11. | Ridley H. Snake venom ophthalmia. Br J Ophthalmol 1944;28:568-72. |
| 12. | Ajao OG, Hawtin JG. Snakebite and snake venom ophthalmia. J Natl Med Assoc 1980;72:961-4. |
| 13. | Lath NK, Patel MM. Treatment of snake venom ophthalmia. Cent Afr J Med 1984;30:175-6. |
Source of Support: None, Conflict of Interest: None
| Check |
DOI: 10.4103/1755-6783.77197
| Figures |
[Figure 1], [Figure 2], [Figure 3]



