| Abstract |
Background : Acute gastroenteritis is a common cause of dehydration and precise estimation of dehydration is a vital matter for clinical decisions. We try to find how much clinically diagnosed scales are compatible with laboratory tests measures. Materials and Methods : During 2 years 95 infants and children aged between 2 and 108 months entered to emergency room with acute gastroenteritis. They were categorized as mild, moderate and severe dehydration, their recorded laboratory tests include blood urea nitrogen (BUN), creatinine, venous blood gases values were expressed by means ±95% of confidence interval and compared by mann-whitney test in each groups with SPSS 16, sensitivity, specificity and likelihood ratio measured for defined cut off values in severe dehydration group, P value less than 0.05 was significant. Result : Severe dehydration includes 3% of all hospitalization due to dehydration. Laboratory tests cannot differentiate mild to moderate dehydration definietly but this difference is significant between severe to mild and severe to moderate dehydration. Conclusion : R outine laboratory test are not generally helpful for dehydration severity estimation but they can be discriminate severe from mild or moderate dehydration exclusively. Creatinine higher than 0.9 mg/dl and Base deficit beyond-16 are specific (90%) for severe dehydration estimation in infant and children.
Keywords: Acute gastroenteritis, children, dehydration, laboratory tests
| How to cite this article: Malaki M. Clinical versus laboratory for estimating of dehydration severity. Ann Trop Med Public Health 2012;5:559-62 |
| How to cite this URL: Malaki M. Clinical versus laboratory for estimating of dehydration severity. Ann Trop Med Public Health [serial online] 2012 [cited 2013 Aug 20];5:559-62. Available from: https://www.atmph.org/text.asp?2012/5/6/559/109262 |
| Introduction |
Acute gastroenteritis is a common reason of hospitalization. [1] It seems that precise diagnosis of dehydration severity may be dependent on laboratory tests, [2] many tried to define dehydration severity with clinically guideline. [3],[4],[5],[6] Capillary refill time, abnormal skin turgor, and respiratory pattern were suggested as the best signs. [7] All these valuable signs may be neither sensitive nor specific for dehydration severity. [8],[9] Clinical dehydration scale (CDS) considers general appearance, eyes changes, mucous membrane moisture and tears existence [10] hospital staying duration can be related to CDS not to laboratory tests (PH and serum bicarbonate) disturbances. With respect to this truth that clinical findings are not sensitive for estimating of dehydration severity solely and importance of laboratory tests results besides to clinical estimation of dehydration grades give more yield for prediction of dehydration severity [4],[5],[8],[11] Yilmaz et al.[12] find serum Urea and bicarbonate can be predictive for dehydration severity in small children and infants as high risk groups to dehydration and We try to find that what laboratory tests can be more compatible for dehydration estimation compared to clinical estimation that can be helpful for physicians in perplexing cases.
| Methods and Materials |
95 children aged between 2 and 108 months diagnosed during 48 month from April 2009 to April 2011 as acute gastroenteritis categorized as mild, moderate and severe with standard criteria [13] by a pediatrician at emergency room. After preparation of laboratory results (blood urea nitrogen, creatinine, venous blood gas, electrolytes include sodium, potassium) these documents evaluated and matched with clinical definition for dehydration severity. Information about age, sex, duration of disease and complaints were asked by a pediatrician residence children height and weight recorded beside to vital signs (blood pressure, pulse rate, respiratory rate and temperature), no one of cases received hypnotic and cholinergic drugs. None of patients had previous diseases like as metabolic disease, renal dysfunction, malnutrition or surgical operation, they affected to dehydration due to acute gastroenteritis in recent days. Their tests include urea creatinine electrolytes (sodium and potassium) venous blood gas (base excess, base, Co2 pressure) weight, height, sex and age of children were also recorded. Serum sodium 135-145 mEq/dl and potassium 3/5-5/5 mEq/dl considered as normal. All results expressed as percent, ratio, means, 95% of confidence interval, minimum and maximum and relation of mentioned laboratory tests in each dehydration severity groups compared by one way ANOVA test and followed by Post-Hoc test of Tukeys test in parametric distribution data for non-parametric ones the mann-whitney test used to compare every two groups individually (mild -moderate), (mild -severe) and (moderate-severe). Four laboratory tests include blood urea nitrogen above 40 mg/dl, creatinine more than 0.9 mg/dl, venous HCO3 below 17 and base deficit beyond to-16 considered as cut off points for severe dehydration and we try to find sensitivity, specificity and positive likelihood ratio(+LR) of these defined values for estimating severe form of dehydration particularly. p was significant if less than 0.05.
| Results |
95 children means age (Minimum, Maximum), 19 months (2, 108) include 29 children with mild dehydration means age (month) ± SD equal to 27±1.5 months, 43 children with moderate dehydration means age ± SD equal to 15±1 and 23 children with severe form aged 14±5 months.
- Average blood urea level ± SD (mg/dl) in mild and moderate were 27±12 and 29±13 these measures were not differed between these two groups (mild and moderate), BUN level in severe form was 49±27 it was higher significantly in severe dehydration compared to mild or moderate dehydration.(P<0.001) [Table 1]. two out of 29 patients with mild, 8 out of 43 with moderate and 11 out of 23 patients with severe dehydration have BUN more than 40 mg/dl (positive LR 3.4, sensitivity %48 specificity 86% for severe form occurrence) [Table 2].
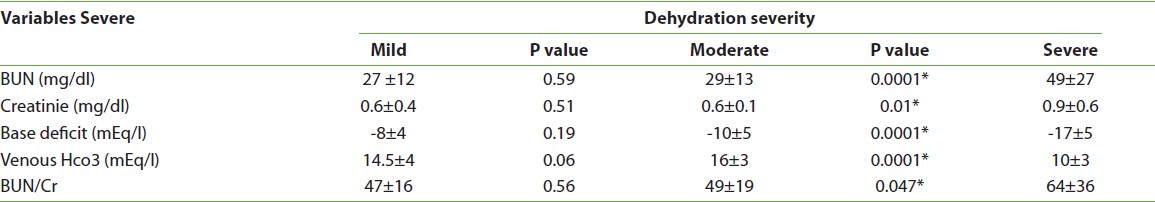
Table 1: Comparison of laboratory tests among three groups of dehydration there is not difference between mild and moderate dehydration but it was significant between severe and moderate /mild forms. (p significant if less than 0.05)
Click here to view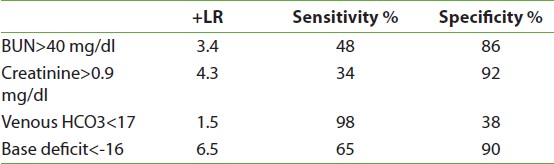
Table 2: Positive likelihood ratio (+LR), sensitivity and specificity of four laboratory tests blood urea nitrogen (BUN), creatinine, venous HCO3, base deficit for predicting of severe dehydration at defined cut off points
Click here to view - Mean ± SD of creatinine (mg/dl) in mild dehydration was 0.6±0.4 while in moderate grade it was 0.6± 0.1 there is not difference between mild and moderate dehydration for creatinine levels but in severe dehydration creatinine level was 0.9±0.6 it was significantly higher in relation to mild and moderate dehydration (p 0.01) [Table 1]. Creaetinine levels above 0.9 mg /dl observed 1 out of 29 with mild, 5 out of 43 with moderate and 8 out of 23 with severe dehydration group (+ LR 4.3, sensitivity 34%, specificity 92% for severe form) [Table 2].
- The mean ± SD (Minimum, Maximum) of BUN to creatinine ratio in mild dehydration was 47±16 (28,100) albeit it was not differed significantly related to moderate dehydration 49 ±19, (30,130)(p 0.56). BUN/Cr was higher significantly in severe dehydration 64±36, (34,170) compare to both moderate and mild dehydration (p 0.04)
- The mean ± SD of venous HCO3 level (mEq/L) in mild dehydration was 16±3 it was not significantly differed to moderate dehydration 14.5±4 (P>0.05) but the mean ± SD of HCO3 was different in severe dehydration 10±3 compare to both mild or moderate dehydration forms (P<0.001) [Table 1].Venous HCO3 measures below 17 mEq/L were observed in 15 out of 29 with mild, 30 out of 43 with moderate and 22 out of 23 patients with severe group (+ LR 1.5 sensitivity 98% specify 38% for severe dehydration form at cut off point of 17 meq/l) [Table 2].
- The mean ± SD of Base excess (BE) decreases significantly (P<0.0001) in severe dehydration compared to mild (-17±5 mEq/L vs-8±4) and moderate dehydration (-17±5 vs-10±5). BE average was not differed between mild and moderate (-8±4 vs.-10±5)(p 0.19) [Table 1]. Base excess beyond to -16 mEq/L has not observed with mild dehydration, it happened in 7 out of 43 with moderate and 15 out of 23 patients with severe group. (+ LR 6.5, sensitivity 65%, specificity 90% in severe dehydration form) [Table 2].
| Discussion |
Attempts to estimate dehydration severity has been done for a long time but using laboratory tests for accurate dehydration severity was noticed recently. [8],[11] Some signs considered as the best tools for dehydration severity. [7] For example losing weight [14] although baseline weights may not be inaccessible and signs like as skin turgor, deep breathing and capillary filling time have some limitations to use for dehydration severity assessment. [7] Urea and bicarbonate level were valuable to predict dehydration severity, serum bicarbonate above 15 can be valuable for mild and moderate dehydration while it occurs infrequently in severe dehydration they consider urea above 100 mg/dl suggestive for severe dehydration although serum bicarbonate below 18 mEq/L is another index that can be used for severe or moderate dehydration estimation. [15] Another study showed that bicarbonate above 15 mEq/L can occur in 7% of severe dehydration episodes. They suggested urea and bicarbonate level can be helpful beside to clinical findings to estimate dehydration severity they suggest that urea level above 100 mg/dl and bicarbonate below 15 suggestive for severe dehydration and urea below 40 and base above 15 are compatible with mild dehydration. [12] Bonedio et al. [2] and Poole (3) suggest serum urea was not predictive for hydration status of dehydrated children while serum bicarbonate was useful for moderate to severe dehydration estimation. In another study on 97 children with acute dehydration Vega and Avner showed that addition of acidosis (bicarbonate <17 mmol/L) to clinical parameters increased the sensitivity for detecting of serious dehydration. [11]
As our study which evaluated serum urea, creatinine, venous base level as HCO3, base deficit and BUN to creatinine ratio in three groups of mild, moderate and severe dehydration, there is not difference in laboratory tests values between mild and moderate dehydration while it was significantly differed among severe dehydration to mild or moderate dehydration in all mentioned parameters (p less than 0.05). To find a cut off point to estimate dehydration severity correctly we found blood urea nitrogen higher than 40 mg/dl is not a sensitive test for diagnosis of severe dehydration condition but its Specificity for severe dehydration is 86%, serum creatinine higher than 0.9 mg/dl was an uncommon finding in mild dehydration but in severe dehydration it was the most specific (92%) finding test. venous base (HCO3) below 17 mEq/L happens in severe dehydration commonly as the most sensitive and the least likelihood ratio test among other tests (sensitivity 98%, +LR=1.5) [Table 2]. Base deficit beyond-16 has an acceptable specificity (90%) and the highest likelihood values (+ LR=6.5) compare to other tests. BUN/Cr ratio higher than 20 occur in all patients and it is not a specific test. As our study clinical estimation of dehydration beside to laboratory tests have more informative for management policies and correct diagnosis in difficult situation if we consider the mentioned cut off points for each tests
| Conclusion |
As our study traditionally clinical dehydration severity estimation is simple and cost effective it seems that routine laboratory tests cannot discriminate mild from moderate dehydration. These tests change significantly in severe dehydration the most sensitive test for severe dehydration diagnosis is the venous HCO3 below 17 mEq/L and the most specific test is creatinine higher than 0.9 mg/dl in the situation with base deficit less than-16 the likelihood ratio for severe dehydration is the highest compare to other identified cut off point laboratory tests.
| References |
| 1. | Pickering LK, Snyder JD. Gastroenteritis. In: Behrman RE, Kliegman RM, Arvin AM, editors. Textbook of Pediatric. 16 th ed. Philadelphia: WB. Saunders; 2000. p. 765. |
| 2. | Bonadio WA, Hennes HH, Machi J, Madagame E. Efficacy of measuring BUN in assessing children with dehydration due to gastroenteritis. Ann Emerg Med 1989;18:755-7. |
| 3. | Poole SR. Criteria for measurement of dehydration. Ann Emerg Med 1990;19:730-1. |
| 4. | Mackenzie A, Barnes G, Shann F. Clinical signs of dehydration in children. Lancet 1989;2:605-7. |
| 5. | Teach SJ, Yates EW, Feld LG. Laboratory predictors of fluid deficit in acutely dehydrated children. Clin Pediatr (Phila) 1997;36:395-400. |
| 6. | Plata Rueda E, Díaz Cruz G. [Clinical and biochemical evaluation of the degree of dehydration in children with acute diarrhea]. Bol Med Hosp Infant Mex 1974;31:561-76. |
| 7. | Steiner MJ, DeWalt DA, Byerley JS. Is this child dehydrated? JAMA 2004;291:2746-54. |
| 8. | Gorelick MH, Shaw KN, Baker MD. Effect of ambient temperature on capillary refill in healthy children. Pediatrics 1993;92:699-702 |
| 9. | Baraff LJ. Capillary refill: Is it a useful clinical sign? Pediatrics 1993;92:723-4. |
| 10. | Friedman JN, Goldman RD, Srivastava R, Parkin PC. Development of a clinical dehydration scale for use in children between 1 and 36 months of age. J Pediatr 2004;145:201-7 |
| 11. | Vega RM, Avner JR. A prospective study of the usefulness of clinical and laboratory parameters for predicting percentage of dehydration in children. Pediatr Emerg Care 1997;13:179-82 |
| 12. | Yilmaz K, Karaböcüoglu M, Citak A, Uzel N. Evaluation of laboratory tests in dehydrated children with acute gastroenteritis. J Paediatr Child Health 2002;38:226-8. |
| 13. | Michael J, Somers G. Clinical assessment of dehydration fluid and electrolyte therapy in children. In: Avner ED, Harmon WE, Niaudet P, Yoshikawa N, editors. 6 th ed., vol. 1, section 2, chap. 13. Berlin, Heidelberg: Springer Verlag; 2009. p. 325-53. |
| 14. | Liebelt EL. Clinical and laboratory evaluation and management of children with vomiting, diarrhea, and dehydration. Curr Opin Pediatr 1998;10:461-9 |
| 15. | Goldman RD, Friedman JN, Parkin PC. Validation of the clinical dehydration scale for children with acute gastroenteritis. Pediatrics 2008;122:545-9 |
DOI: 10.4103/1755-6783.109262
| Tables |



