This review evaluates the National Tuberculosis and Leprosy Control Programme (NTBLCP) of Nigeria to identify challenges and prospects for reducing the burden of tuberculosis (TB) in Nigeria. Keywords: Evaluation, national tuberculosis and leprosy control programme, Nigeria, review Key messages: Rates of TB morbidity and mortality in Nigeria are spiralling despite expressions of political will to control TB and a clearly articulated TB control policy. Following review and analysis of these TB control strategies, progress can be achieved by building upon existing resources while fostering stronger partnerships with relevant organizations.
Tuberculosis (TB), an ancient infectious disease caused by Mycobacterium tuberculosis, is the leading cause of death due to an infectious agent globally. It is both preventable and treatable. [1],[2] TB is a disease of poverty affecting mostly young adults in their most productive years and reduces an individual’s capacity to work. [3],[4] Globally, there are more cases of TB today than in previous epochs of human history. The World Health Organization (WHO) records an average of 9 million new TB cases annually and about 5,000 TB deaths daily. [1] It is projected that by the year 2050, the annual death rate from TB will exceed 5 million a year. [5] TB and Human Immunodeficiency Virus (HIV) co-infection and the exponential increase in multidrug-resistance are greatly responsible for TB assuming almost epidemic proportions. [5],[6] Challenges which are peculiar for TB control in Sub-Saharan Africa are poverty, weak political will and weak health systems, inadequate human resources and poor laboratory services. [4],[7] TB is a major public health problem in Nigeria and it was declared a national emergency in 2006. [8] Following the Abuja Declaration in 2001, Directly Observed Therapy Short course (DOTS) activities have been scaled up across Nigeria. In spite of the documented effectiveness of DOTS in the Nigerian context, [9] Nigeria has the tenth largest burden of TB cases in the world. [10] The 2012 WHO estimates for Nigeria put the prevalence of TB at about 280,000 (171 per 100,000) cases with an incidence of 190,000 (118 per 100,000) and a mortality of 27,000 (17 per 100,000). [11] The Case Detection Rate (CDR) was low at 45% while the Treatment Success Rate (TSR) among new smear-positive cases for 2010 was 84%. In 2011, there were 95 laboratory confirmed cases of MDR-TB in Nigeria. [11] Despite expressions of political will to control TB and a clearly articulated national TB policy, neither the set target for CDR nor cure rates has been achieved nationally. TB continues to account for high rates of morbidity and mortality within Nigeria in spite of reports of 99% geographic coverage using the DOTS strategy by 2008. [8],[11] This situation has been further compounded by the high HIV prevalence of 4.1% in Nigeria. [12] Nigeria accounts for about 10% of the total global burden of HIV with estimates of 3.4 million people living with HIV by the end of 2011. [12] This review analyses the NTBLCP services in a bid to identify challenges and prospects for reducing the burden of TB in Nigeria.
A literature search was conducted from November 2011 to March of 2012. Thus, secondary data was utilized from documents from NTBLCP of Nigeria, databases (PubMed, Popline, Global Health, Medline and Web of Science), organizational websites and search engines (Google Scholar and Scirus) were used. The search was executed in two steps. In the first step, an initial individual keyword search was done. Keywords were then combined using the Boolean characters “AND” to limit search results. The keywords included: “Tuberculosis” AND “National Tuberculosis Control Programme” AND “Nigeria.” In the search for international literature, the keyword “Nigeria” was excluded. Reference lists of identified articles were then searched further for relevant reports. In the second step, sort criteria were applied to obtain more relevant articles. This entailed selection of relevant titles and further reading of abstracts with scanning and skimming. This narrowed the number of articles and the full length versions were read. A total of 49 articles were eventually used in this review. A Zetoc alert list was also created; peer reviewed journals such as the International Journal of Tuberculosis and Lung Disease and British Medical Journal were subscribed to. An email alert was set up to receive any updates. The following inclusion criteria were considered: i. English Language: Only articles written in English language were used to avoid translation errors and misinterpretation. ii. Peer reviewed vs. non peer reviewed articles: Peer reviewed articles were also preferred because of the authenticity of their content iii. Literature relevance to research question: The article titles and abstracts were scrutinized to ensure that the contents were related to the research question. iv. Publication dates: Articles published in the previous 10 years were preferred because their information was more current and relevant.
Information derived from the search is discussed below. Nigeria has 36 States, a Federal Capital Territory and 774 Local Government Areas (LGA) as shown in [Figure 1]. With a projected population of 152 million, Nigeria is the 4 th largest country in Africa [13] and approximately 70% of Nigerians reside in rural areas. [14] There is a high prevalence of the wider determinants of TB among Nigerians; these include poverty, smoking, malnutrition, ignorance, overcrowding and living in poorly ventilated houses. [15] This promotes inequality as poor communities in Nigeria are more affected by hidden costs of TB care and are thus less likely to access health services. [3]
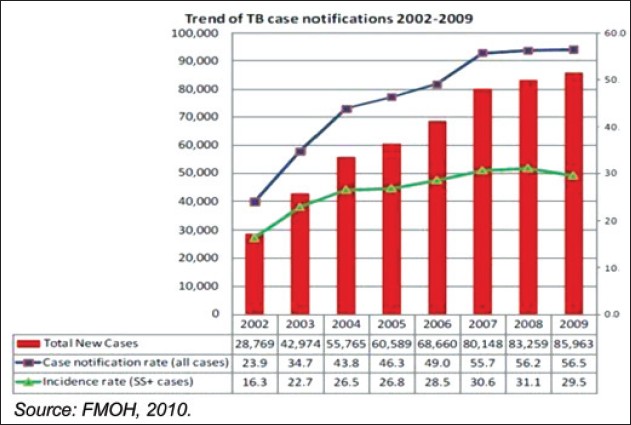
NTBLCP of Nigeria was officially launched in 1991 with a mandate to coordinate TB and Leprosy Control activities in the country and reduce the burden of both diseases. [8] This review focuses on the TB control component of NTBLCP of Nigeria. The NTBLCP is structured along the three tiers of government i.e. Federal, State and LGAs. [8] Its activities are supported by development partners. Prominent among these are WHO, Global Fund to fight AIDS, TB and Malaria (GFATM), International Union Against Tuberculosis and Lung Diseases (IUATLD) and United States Agency for International Development (USAID). There is a National TB training centre in Zaria which is responsible for development of human resource, training guidelines and operational research relating to TB. [16] The basic strategy of NTBLCP remains the provision of free DOTS to all persons with active TB. Supportive strategies are outlined in the new Strategic Plan (2010-2015) which has the following components: i. Improving key indicators such as CDR and TSR via quality assured bacteriology. ii. Pursuing high quality DOTS expansion and enhancement. iii. Addressing TB/HIV co-infection. iv. Controlling MDR-TB. v. Provision of laboratories and quality assurance services. vi. Increased and sustained funding for TB control. vii. Engaging people with TB and affected communities via ACSM. viii. Involving all care providers through PPM. The analysis of NTBLCP activities will focus on these components. Key Indicators of TB Control in Nigeria There have been rising trends in TB incidence and case notification rates over an eight year period (2002 to 2009) as depicted in [Figure 2]. These rising trends may be related to rising rates of HIV infection and MDR-TB in Nigeria. [17] The high prevalence of socio-demographic determinants of TB in Nigeria and population growth may likely have a contributory role. NTBLCP efforts have yielded results as depicted in [Figure 2] by doubling of smear positive CDR from 16.3% in 2002 to 31.1% in 2008. However, these indicators of NTBLCP good performance appear to be overshadowed by the exponential increase in total number of new cases of TB.
Case notification rates have been shown to vary from one state to the other with Kwara State having the least rate (900 per annum) when compared with other states in the country like Lagos (8200 per annum) and Oyo (6000 per annum). [18] Interestingly, the percentage of smear positive among new TB cases has fallen in recent years as seen in [Figure 3]. These findings are corroborated by a study on trends of tuberculosis notification in Ebonyi, south-eastern Nigeria that observed a progressive increase in the proportion of smear-negative pulmonary tuberculosis (PTB) during 2003 to 2009. This was associated with a concomitant continuous reduction in the proportion of smear-positive PTB. [7] This exact trend has been reported nationally. [19]
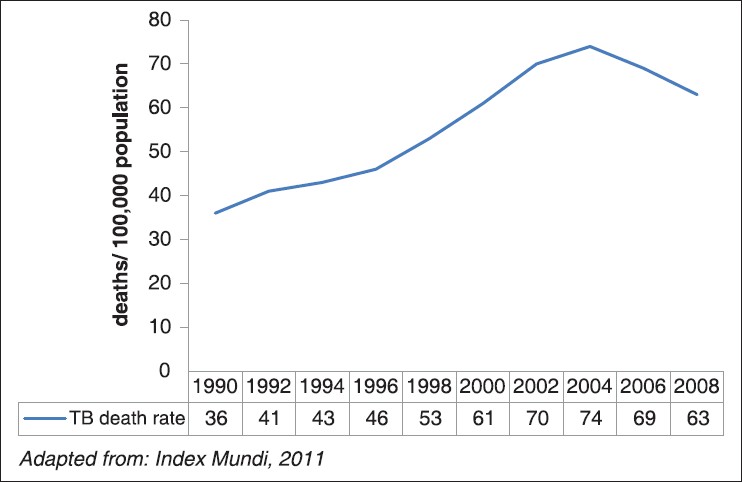
A review of TB mortality rates in Nigeria over a 19 year period showed a gradual rise from 1990 to 2004 as illustrated in [Figure 4]. From 2004, TB mortality rates dropped steadily till 2008. This coincides with the adoption of WHO STOP TB strategy by NTBLCP. This decrease in TB mortality rates in the face of rising incidence rates is highly suggestive of improvements in TB care. This improvement is also reflected in an increase TSR; TSR of smear positive TB cases increased from 73% in 2004 to 83% in 2009. Eleven States achieved the minimum of 85% TSR in 2009. [13] All these suggest concerted effort by NTBLCP to control TB.
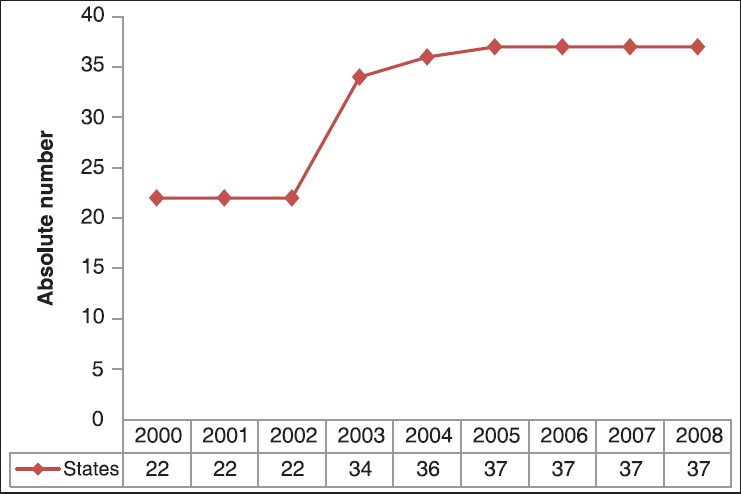
DOTS Expansion The DOTS strategy was introduced in southern Nigeria about a decade before it was started in northern Nigeria. [20] Since DOTS was introduced in northern Nigeria, about 65% of the total national TB case notification during 2002 to 2007 came from the region. [20],[21] There has been a progressive increase in the number of DOTS centres in Nigeria over the last decade as illustrated in [Figure 5] and [Figure 6]. DOTS coverage serves as a proxy for people with access to DOTS. [22] Currently, Nigeria has a total of 3,459 functional DOTS centres with a ratio of 1:43,943 as against the NTBLCP target of 1:25,000 population. [13] The South West region has the highest number of sites (754) with North East having the least (426) as shown in [Table 1]. This reflects inequality as the poorer northern states have fewer TB centres per capita. [3] The 100% DOTS coverage achieved in 2004 is rather deceptive and masks the fact that many LGAs are yet to be covered. [3]
Shortage of skilled TB health workers at PHC level and financial constraints has impeded the successful implementation of DOTS in Nigeria. [3],[23] This has resulted in inequalities as a large proportion of the population remain underserved by TB care services. The alternative patient centred approach to TB control especially community based DOTS is yet to properly take off in the country. [24] Although the NTBLCP recognise the need to elicit the support and participation of community members in TB control efforts, this is yet to be reflected in its activities. [24] Incentives for patients and DOTS providers are also lacking in the Nigerian TB control system. [24] Factors most commonly linked to inaccessibility of TB services in Nigeria include distance, time, money and knowledge about where to obtain services free-of-charge. There have been reports of clients travelling a distance of 40 kilometres every day within a State to receive treatment. [3] Accessibility is further limited by the centralization of TB control activities with less activity in rural areas. [25] This places many Nigerians who reside in rural areas at a disadvantage. Men have been shown to utilize TB care services more than the womenfolk in Nigeria. [26] This may be linked to cultural factors which allocate more power to men and gives lower priority to the health of women. Laboratory and Quality Assurance Services As at 2009, Nigeria had a national reference laboratory and 1025 other laboratories providing TB microscopy services. [13] A critical look at the distribution of microscopy centres in relation to the projected population for 2009 shows a ratio of 1: 149,000 as against the NTBLCP target of 1: 80,000 populace, giving a shortfall of 47% population target coverage. Of the 774 LGAs, 670(87%) have functional sputum microscopy facilities. However, only three centres in Nigeria offer automated BACTEC TB culture and drug susceptibility testing (DST); the six zonal reference culture laboratories are yet to be fully operational. [26] This falls short of the WHO recommendation of 1 culture facility per five million population. [27] Nigeria lacks an external quality assurance (EQA) system for its laboratories. [23] There are also insufficient skilled laboratory personnel; Nigeria has approximately 0.005/1000 population laboratory technicians which is far below the 0.031/1000 population laboratory technicians required to ensure accessibility to TB microscopy. [23] The NTBLCP training centre which provides TB laboratory courses appears to be underutilized. [16] This poor state of TB laboratories in Nigeria has been attributed to poor financing and low prioritization. [3] TB/HIV co-infection The high incidence of HIV infection in Nigeria has significantly increased TB cases. Also, poor adherence to anti-TB medications which predisposes to MDR-TB has been shown to be significantly higher among HIV-positive persons in Nigeria. [28] In a bid to identify cases of co-infection early, NTBLCP is working to increase the proportion of TB patients tested for HIV from 62% in 2008 to at least 85% by end of 2015. [13] There has been progress in this direction as WHO reported that 75% of Nigerian TB patients in 2009 knew their HIV status as shown in [Figure 7]. Also, TB/HIV co-infection rates were reported to be as high as 26% with only 39% of HIV positive TB patients started on ART. [1]
The National Policy on HIV/AIDS explicitly emphasizes the need to provide a comprehensive continuum of care for people living with HIV/AIDS. [29] This has promoted linkages between NTBLCP and National AIDS and STDs Control Programme (NASCAP). The NTBLCP has promoted TB/HIV collaborative activities with the strategic aim of reducing by 25% the HIV infection rate among TB patients and the TB incidence among HIV-infected persons. [3] However, there are barriers to establishing integrated TB/HIV services in Nigeria. Firstly, many HIV clinics in Nigeria still operate passive case finding approaches for TB by screening only patients with symptoms suggestive of TB. [30] Secondly, many TB clinics do not possess the equipment for early diagnosis of TB among TB/HIV co-infected persons. Thirdly, there has been a display of “territoriality” with a seeming reluctance among health workers in TB and HIV care to collaborate. [3] Fourthly, there appears to be a lack of knowledge on the limitations of the existing diagnostic tools and the more current alternatives among clinicians. [31] Lastly, there is a lack of human and financial resources to strengthen this linkage and make it more effective. [3] MDR-TB The relatively low TSR for TB in Nigeria raises serious concerns about the elevated risk of an MDR-TB upsurge. However, NTBLCP has been mainly focused on DOTS and currently has no separate line budget for managing MDR-TB. [3] Guidelines for programmatic management of MDR-TB have been developed but MDR-TB treatment programs are in the nascent stages. Treatment of MDR-TB involves use of second-line drugs, which are costly, scarce, toxic and require longer durations of therapy. [32] A few private hospitals offer second-line drugs at a cost of between $5,475 (NGN 731,000) and $10,000 (NGN 1.3 million) per patient annually, putting these drugs out of the reach of most Nigerians and promoting inequality. [3] The six zonal MDR-TB testing and treatment centres proposed by GFATM in collaboration with NTBLCP are yet to be fully operational. This accounts for the absence of MDR-TB patients on treatment despite the confirmation of 28 cases of MDR-TB in 2009 as shown in [Table 2].
The slow development of MDR-TB services in Nigeria may be linked to the capital intensive nature of required facilities and weak collaborations with development partners. Due to a lack of research into the pattern of MDR-TB strains in Nigeria, the ideal second line combination remains largely unknown. There is also a lack of representative surveillance data on MDR-TB and there are no concrete arrangements in place for recording and reporting for MDR-TB. Lastly, human resource capacity for management of MDR-TB is very limited. [3] Funding for TB control The proportion of total TB funding needs covered by national governments is a key indicator of political commitment. [33] The political commitment exhibited by the Nigerian government has not yet been translated into adequate budgetary allocations for TB control. This is reflected in [Table 3] with GFATM making the highest contribution to TB control in Nigeria. This underfunding has compromised the capacity of the health system to tackle the growing TB burden. [3] This has resulted in reluctance on the part of external donors to fund TB control in Nigeria in the face of limited government funding. [17] There have also been challenges with ensuring that approved government funding for TB control is released for use. States and LGAs have demonstrated a low level of commitment and financial accountability to TB control. The States and LGAs have repeatedly failed to pay their share of funding agreed upon in memoranda of understanding with donor organizations. [3] All this has contributed to the huge financial gap that exists between the proposed budgets and available funding of NTBLCP.
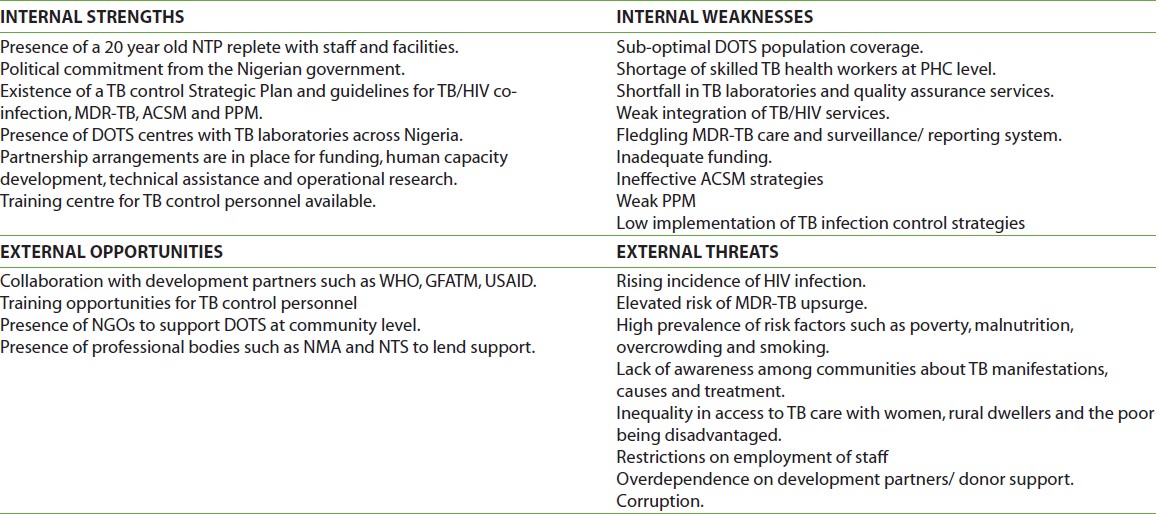
ACSM Guidelines for ACSM in Nigeria were developed by NTBLCP in 2008. [13] Mass media advocacy for TB control has been done through airing of jingles, health talks on TB and publishing articles on TB in newspapers. Advocacy committees have been established at State and LGA level. Poorly co-ordinated attempts have been made to engage civil society organizations and community and religious leaders. However, all these efforts at promoting ACSM have lacked articulation and sustainability. Also, NTBLCP staffs have little training on skills necessary for working with the press. [3] This largely ineffective ACSM strategy in Nigeria has resulted in a lack of awareness among communities about TB. [17],[34] It has also contributed to high levels of stigma and discrimination against people living with TB with resultant social inequality. [3],[35] PPM PPM consists of strategies that link all healthcare providers within the private and public sectors to NTPs for expansion of DOTS. [36] In low medium income countries, it has been shown that people across socio-economic strata with tuberculosis are likely to present first to a private practitioner for care. [37] In Nigeria, it’s estimated that up to 60-70% of TB care is provided by private practitioners. It was discovered that Nigerians were more likely to seek TB care from between two to six providers before coming to DOTS centres. [25] These private practitioners were less likely to follow the national treatment guidelines. Their prescription of anti-TB drugs appeared to be based on the purchasing power of clients rather than NTBLCP guidelines. [3] Also, only few private practitioners referred TB patients to public health facilities or reported on the cases they treated and there was considerable delay beforereferral. [5] As private practitioners charge user fees, TB treatment was restricted to those who can afford these services thereby promoting inequality. [3] NTBLCP of Nigeria has made progress in achieving PPM. The national PPM situation assessment was carried out in 2007 followed by the development of national PPM guidelines. In 2009, health development committees were set up in 12 hospitals. Also, steering committees were inaugurated in five additional states in 2009 to oversee the phased implementation of PPM DOTS. This brought to 11 the number of states practicing PPM DOTS. However, the other 25 states are without PPM DOTS schemes. [13] Barriers to PPM in Nigeria exist within NTBLCP and in the private medical sector. Barriers within NTBLCP include lack of information on the private sector, preoccupation with expanding DOTS and weak regulatory mechanisms. Barriers within the private medical sector include inadequate training and lack of information, infrastructural limitations to performance and disorganization. [38] A study by Okeke et al., in Enugu Nigeria reported that though private practitioners were keen on receiving information on TB management, only few of them had ever participated in any continuing medical education programme on TB. Even fewer had been contacted by the NTBLCP on TB management issues. [37] TB Infection control Transmission of M. tuberculosis is a recognized risk in health-care facilities. The transmission could be to patients, visitors or health care workers. [39] The NTBLCP of Nigeria has adopted international best practices with regards to infection control for TB. [40] This three level hierarchy consists of administrative (managerial) control measures/ work place policy, environmental control measures, and use of personal protective equipment. Ogbonnaya et al., in a descriptive study triangulated self-administered questionnaires with review of facility case notes and participant observation techniques to assess TB infection control in twelve health facilities in Southern Nigeria. [41] They found very low implementation rates of between 8.3%-41.7% of various aspects of the administration control and work practice components of TB infection control. No facility had Information, Education and Communication (IEC) materials reminding patients and health workers about the risk of acquiring TB from health facilities. Most of the health facilities in this study were not implementing any components of the three levels of TB infection control. There was no periodic screening of health workers with Mantoux test. TB patients were found to be nursed in the same ward with other vulnerable patients like those infected with HIV. [41] The findings of this study may be a reflection of the state of infection control in Nigeria. The Strength Weaknesses Opportunities and Threats (SWOT) analysis in [Table 4] summarises all these findings.
In a bid to strengthen TB control in Nigeria, it may be pertinent to review some effective strategies for improving TB control across the globe. Expansion of DOTS has been linked to increases in TB CDR. [42] Expanding DOTS coverage from 0% to 100% of the population has been shown to raise mean TSR by 18%. Countries studied included Botswana, Indonesia, Korea, Lesotho, Namibia, Philippines, and South Africa. [43] In a bid to rapidly scale up DOTS coverage, the NTPs of Bangladesh, Thailand and Tanzania have introduced successful and innovative community-based DOTS programmes, in collaboration with NGOs. In Bangladesh, the lack of capacity to administer DOT through health care workers in every community has been addressed using Bangladesh Rehabilitation Assistance Committee (BRAC). BRAC is the largest NGO in Bangladesh with over 70,000 health volunteers. BRAC now provides community-based TB services in over two-thirds of the country through female community workers (Shastho shebikas). [3] These workers are trained to identify symptoms of TB and refer suspected cases for TB diagnosis within their community. They then collect free anti-TB medications for diagnosed cases and administer them at household level. Shastho shebikas receive regular training and refresher courses. As incentives, they receive a small fee for each TB patient and are permitted to sell pharmaceutical supplies in their communities. [3] The BRAC has successfully achieved TSR above the global target of 85% at cost 50% less than equivalent services covered by the NTP. They have also defused stigma by raising awareness on TB. [44],[45] The guiding principles of TB/HIV integrated care include testing all TB patients for HIV, screening all HIV patients for TB, providing anti-retroviral drugs early for HIV patients to reduce the incidence of TB, and provision of isoniazid preventive therapy for HIV persons at high risk of TB. It also requires close proximity of TB and HIV service delivery points. [46] In settings with high TB/HIV co-infection, active efforts to identify undiagnosed TB do produce high yields. This was found in settings as diverse as Cambodia, Haiti and South Africa where between 4 to 9% of active undiagnosed TB was discovered among HIV-positive persons. [47] They utilized active screening for TB in settings that concentrated HIV-infected persons such as hospitals, HIV testing and counselling centres and prisons. In Khayelitsha sub-district of South Africa, integration of TB/HIV care services was achieved; both services were provided within the same facility. This resulted in increased HIV testing of TB patients from 30% to 56%, with 87% of those offered accepting testing, in contrast to 8% and 40% in a similar township without integration. [48] Referral delays and loss to follow-up of co-infected persons reduced with earlier treatment initiation. Also, monitoring of treatment improved with better clinical awareness of drug interactions and side effects. Cross-training of TB and HIV care workers was accomplished causing both to be able to rotate between services. The resulting increase in competence led to an increase in staff morale. [49]
Examining the context within which NTBLCP operates helped to identify the challenges and prospects for achieving TB control in Nigeria. Complete DOTS population coverage is yet to be achieved, there is a weak integration of TB/HIV care services and MDR-TB management is still at the nascent stage. Other issues are inadequacy of laboratory and quality assurance services, wide funding gaps and ineffective ACSM and PPM. There is also a low implementation of TB infection control strategies in health care settings. Prospects for TB control in Nigeria include the existence of a 20 year old NTP replete with resources and guidelines for achieving the various STOP TB targets. Others are the presence of political commitment by the Nigerian government, abundance of NGOs and willingness of various development partners such as the WHO and GFATM to assist. Harnessing the above potentials while addressing systemic weaknesses will be a bold step towards ameliorating the burden of TB in Nigeria. The applicability of some of the effective TB control strategies identified above to the Nigerian context needs to be explored in greater detail.
Source of Support: None, Conflict of Interest: None
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7]
[Table 1], [Table 2], [Table 3], [Table 4] |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||