| Abstract |
Actinomycosis is a chronic, suppurative disease characterized with granulomatosis and fibrosis. Although it causes oral and cervicofacial infections generally, in 20% of cases it is abdomino-pelvic located. A 24-year-old male patient was examined with the diagnosis of diaphragm, adrenale and chest wall-invasive mass in liver vault. Exploration and mass excision were made with pre-diagnosis of liver tumor and the pathologic result of the patient was reported to be Actinomyces infection. Having no problem in the post-operative period, patient was discharged following the arrangement of antibiotic treatment.
Keywords: Actinomyces, liver, thoracotomy
| How to cite this article: Kerem M, Celik A, Erdem O, Tastepe I. Local invasive Actinomyces infection mimicking liver tumor. Ann Trop Med Public Health 2013;6:567-8 |
| How to cite this URL: Kerem M, Celik A, Erdem O, Tastepe I. Local invasive Actinomyces infection mimicking liver tumor. Ann Trop Med Public Health [serial online] 2013 [cited 2016 Mar 24];6:567-8. Available from: https://www.atmph.org/text.asp?2013/6/5/567/133720 |
| Introduction |
As an opportunistic pathogen, Actinomyces generally occurs as oral cavity or cervicofacial infection in 50% of cases. Although liver and other abdominal organ involvements and pelvic involvement are rare, they can be generally seen pursuant to the hematogenous spread of current infection or performed gastrointestinal-pelvic interventions and/or surgeries. [1] Despite advanced imagining techniques, it is hard to diagnose cases with isolated intra-abdominal organ involvement as culture results are generally negative. For that reason, cases are pathologically diagnosed following the exploration.
| Case Report |
The present case report is about a 24-year-old male patient who was examined with the complaint of the right side pain existing for 2-3 months. Having tooth extraction history, the patient’s physical examination and routine blood values were normal. In abdomen computed tomography (CT), approximately 3.5 × 5.5 sized mass lesion is detected in left subdiaphragmatic region [Figure 1]. Tumor markers of the patient were normal and increased activity value (Suv max:12) was detected at liver segment 6 level with positron emission tomography CT. Liver needle biopsy was not diagnostic. For that reason, it was decided to perform surgery on the mass, surrounding tissues and fat plans of which could not be recognized in tomography. Having been consulted to thoracic surgery department due to possible chest wall invasion, the patient underwent the surgery. In the surgery, thorax was opened from 7 th intercostal range with right posterolateral thoracotomy. Pursuant to frenetomy, 5 cm lesion placed in liver segment 6 was reached and the mass was excised from liver tissue. Then, 11-12 th costas were partially resected and the mass was excluded en bloc with adrenale tissue. The defect in diaphragm and chest wall was repaired primarily. In incisions which were prepared with liver resection material, neutrophil characterized granuloma structures, mid of which is in necrotic appearance are observed between mononuclear cells and fibrosis characterized inflammatory focuses. Microorganisms were observed to be compatible with Actinomyces which were stained histochemically with gram + Browm Brenn stain [Figure 2]. Pathology result was reported to be Actinomyces infection having gram (+), antimicrobial-resistant bacteria (−) staining features. Having no problem in the post-operative period, patient was discharged and conditioned to complete doxycycline 100 mg 2 × 1 capsule treatment within 6 months.
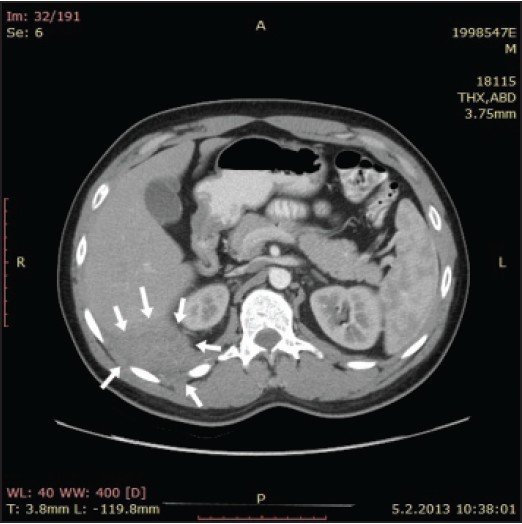 |
Figure 1: The mass which is observed to have heterogeneous contrast involvement following the central necrotic intravenous contract injection, cannot be distinguished from intercostal muscle plans and diagram in computed tomography
Click here to view |
| Figure 2: (a) Neutrophil characterized granuloma structures, mid of which is in necrotic appearance (H and E, ×100) (b) Microorganisms compatible with Actinomyces stained histochemically with gram + browm brenn stain
Click here to view |
| Discussion |
Actinomyces is a rare infection, which is frequently observed in developing countries. 6 of 13 defined types of Actinomyces are found in human as pathogen. [1] Among these types, the most isolated one in human is Actinomyces Israelii, which is found in normal mouth flora and gastric aspirate. Mostly seen as head and neck infection, this pathogen may appear as secondary intraabdominal organ involvement following intraabdominal surgery/interventions or in thoraco-abdominal infections. Pelvic infection and abscess formation related to this pathogen are defined especially in women using intrauterine contraceptive device. In addition, in patients with biliary and pancreatic stent, intraabdominal foreign substances are a risk factor for such infections. Liver involvement is seen as hematogenous spread through portal ven from another focus or neighborhood spread. Primary liver involvement is at the rate of 5%.
Clinically, Actinomyces infections appear as subfebrile fever, anorexia, weight loss, anemia, malaise and localized. [2] In colon located cases, constipation; in mediastinum located cases, dyspnea and post-pericardium fistula tamponade; in liver periphery located cases, skin fistula are reported. [3],[4],[5]
Histopathological and culture examinations are important for diagnosis. Actinomyces is a Periodic acid-Sciff (+) and gram (+) bacteria. However, histopathologically it may have similar appearances as nocardia, aspergillosis, cephalosporium and some staphylococcals. In general, appearance of sulfur granules is important for the diagnosis of Actinomyces. It might be possible to diagnose by means of the histopathological and culture samplings of aspirates obtained from lesions which are placed in the appropriate location for needle biopsy. [3] However, culture results are negative in 76% of cases. [6] In addition, radiological examinations appear as hepatic abscess or liver mass. [1],[4],[6]
Due to the non-specific clinic, radiologic and laboratory results, final diagnosis of Actinomyces infections is made following the surgical exploration in most cases. Cases with primary liver involvement can be interpreted to be with a tumor on condition that no other focus is found or no finding appears related to Actinomyces infection. [1],[4]
For medical treatment of diagnosed patients, high dose penicillin G (10-20 million unit/day) is applied as intravenous for 2-6 weeks. Then, oral treatment continues with phenoxypenicillin as 2-4 g/day for a few weeks. [2] Moreover, antibiotics such as doxycycline, tetracycline, clindamycin and erythromycin are also effective on bacteria and can be used for 4-6 months orally.
| References |
| 1. | Wayne MG, Narang R, Chauhdry A, Steele J. Hepatic actinomycosis mimicking an isolated tumor recurrence. World J Surg Oncol 2011;9:70. |
| 2. | Lee JD, Kim PG, Jo HJ, Park DH, Seo EJ. A case of primary hepatic actinomycosis. J Korean Med Sci 1993;8:385-9. |
| 3. | Saad M, Moorman J. Images in clinical medicine. Actinomyces hepatic abscess with cutaneous fistula. N Engl J Med 2005;353:e16. |
| 4. | Filippou D, Psimitis I, Zizi D, Rizos S. A rare case of ascending colon actinomycosis mimicking cancer. BMC Gastroenterol 2005;5:1. |
| 5. | Sakaguchi Y, Isowa N, Nakazaki H, Takeda K, Tokuyasu H, Saitoh Y, et al. Acute cardiac tamponade caused by the extension of multiple hepatic actinomycotic abscesses. Intern Med 2012;51:305-8. |
| 6. | Acquaro P, Tagliabue F, Confalonieri G, Faccioli P, Costa M. Abdominal wall actinomycosis simulating a malignant neoplasm: Case report and review of the literature. World J Gastrointest Surg 2010;2:247-50. |
Source of Support: None, Conflict of Interest: None
DOI: 10.4103/1755-6783.133720
| Figures |
[Figure 1], [Figure 2]



