The common perception and belief among general medical fraternity about vivax malaria is its benign nature and rare association with any known complications. Even, the literary evidence is scarce regarding the devastating complications of malaria due to vivax but is abundant with complicated reports of falciparum malaria. Therefore, any such complicated case of vivax malaria throws diagnostic challenges to the attending physician and is very difficult to exclude the presence of other type of infections and falciparum infestation. Among various complications associated with malaria, pulmonary complications are rare and the possibility of acute respiratory distress syndrome (ARDS) is even rarest with vivax infection. The present case is a description of rare pulmonary complication of vivax malaria resulting in ARDS and its successful management. Keywords: Acute respiratory distress syndrome, malaria, Plasmodium falciparum, Plasmodium vivax
Among Asian countries, Indian subcontinent is a highly endemic area for malaria. The mortality and morbidity associated with complications of malaria have always been the cause of worry for the attending physician and the intensivist. The bite of female anopheles mosquito is responsible for the transmission of malarial parasites to human body. [1],[2] The disease can present in a diverse form and the symptomatology associated with malaria can have both typical and atypical presentations. Half of the endemic prevalence in Asian countries is largely due to Plasmodium vivax among the four malarial species. The typical symptoms of malaria include but are not limited to onset of fever with chills and rigors, headache, weakness, vomiting, and diarrhea. However, untreated and partially treated cases can progress to develop severe form of complications such as acute renal failure, disseminated intravascular coagulation, acute respiratory distress syndrome (ARDS), hypoglycemia, coma, or epileptic seizures. This wide spectrum of disastrous complications is seen more often with Plasmodium falciparum and is rarely associated with P. vivax. Among the various complications associated with malaria, pulmonary complications can be seen in approximately 4-18% of all the cases suffering from malaria. As such, ARDS and pulmonary edema can be seen with P. falciparum infestation and on rare occasions with infection due to other species including P. vivax. [1] We report a case of ARDS complicating infection with P. vivax malaria.
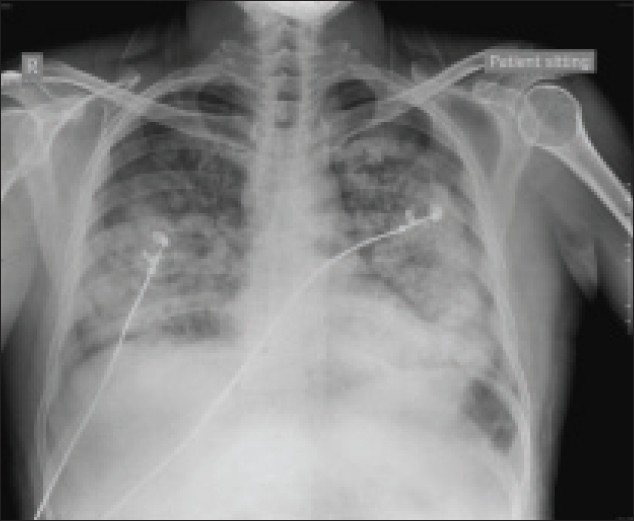
A 33-year-old male patient was admitted to medicine emergency ward with history of fever, chills, and rigors intermittently for the last 7 days. He also had multiple episodes of vomiting and loose stools for the past 1 week. There was also one episode of altered sensorium about 5 days back, which lasted for few hours. On elicitation of detailed history, it was revealed that patient did not have any positive history of systemic medical illness including hypertension and diabetes mellitus. He was referred from a small nursing home after being given the primary symptomatic treatment and his medical record showed that he had weak, thready pulse and BP of 90 mmHg systolic. Patient was referred to the tertiary care center for further management. On initial examination during admission, he was conscious and oriented, and general examination revealed a fever of 102.2 F with rigors and chills, mild hypotension (98/54 mmHg), a pulse rate of 98 beats/min, and a respiratory rate of 28/min. Complete hemogram, renal function test, liver function test, and other requisite investigations were carried out. Empirical antibiotic therapy was started with ceftriaxone in the form of injection. Peripheral blood smear was sent for examination for malarial parasites as the symptoms also pointed toward the possible infection with malaria. In lieu of deteriorating hemodynamic parameters, infusions of dopamine and dobutamine were started and the patient was shifted to intensive care unit (ICU) for further management. Along with fever, patient was also suffering from mild jaundice and had tenderness over right hypochondrium. A provisional diagnosis of cholangitis was confirmed by the Ultrasound report revealing cholelithiasis. Inj. piperacillin and tazobactam combination and inj. metronidazole were added to the therapeutic regimen. Meanwhile, peripheral blood smear confirmed the presence of P. vivax infection. Patient was injected with quinine 500 mg infusion 6 hourly administered over 2-3 hours. Rest of the investigations revealed a decreased platelet count (10,000/mm 3 ) and a total leukocyte count of 14,200/cumm. Blood culture and urine culture were sterile, whereas Widal test and viral markers were negative for hepatitis and HIV. Two days after admission, patient had acute onset of dyspnea with respiratory rate increasing to 32-38/min. Auscultatory findings revealed a grossly decreased air entry in basal areas of chest and presence of fine basal crepitations bilaterally. Patient was kept in propped up position and oxygen supplementation was administered with venturi mask during the initial period. Nebulization was carried out with salbutamol and steroids. However, in spite of these entire measures, patient’s clinical status kept on deteriorating progressively. Chest X-ray revealed bilateral fluffy opacities [Figure 1]. Patient’s respiratory system showed gradual but progressive deterioration as evident by a falling oxygen saturation to 95-96% on pulse oximetry even with oxygen supplementation with venturi mask. Neither noninvasive ventilation nor endotracheal intubation could be performed during this period as the patients’ relatives did not give consent for the same. Moreover, involvement of accessory muscles of respiration and gradually increasing respiratory rate, which was fluctuating between 30 and 45/min, was a serious concern. Arterial blood gas (ABG) analysis revealed pH value of 7.47, PO 2 of 57 mmHg, and PCO 2 of 28 mmHg. In anticipation of impending respiratory failure and after convincing the patients’ relatives about the prognosis without intubation, patient was intubated and put on mechanical ventilation after administering propofol, succinylcholine, and midazolam.
Patient was sedated and paralyzed and kept on control mode of ventilation. Central venous access was secured for guidance of fluid administration with a goal to achieve a central venous pressure of 8-10 cm of H 2 O. ABG was done after 2 hours and revealed a pH of 7.28, PO 2 of 62 mmHg, PCO 2 of 45 mmHg at 70% of oxygen supplementation, and positive end expiratory pressure (PEEP) of 8. After consultation with the physician and considering the current clinical status, a diagnosis of ARDS was made. Ventilator strategies were formulated and settings were adjusted to low tidal volume (LTVS) with a higher PEEP, which was gradually increased to have an acceptable ABG, with maximum PEEP of 12. Further, fresh investigations revealed an increased bilirubin level of 5 mg% and a serum creatinine value of 3.5 mg%. In spite of high creatinine values, hourly urine output was 50-60 ml/hour. High creatinine value was probably due to initial dehydration and hypovolemia, which subsequently improved with adequate i.v. fluid management. As such, patient did not require renal replacement therapy throughout his stay in the hospital. Blood sugar levels were also high on serial monitoring and a gradual normoglycemia was achieved with regular insulin infusion. After 48 hours of LTVS ventilation, patient condition gradually improved as was evident from the analysis of ABG report, which revealed a pH of 7.37, PO 2 of 110 mmHg, and PCO 2 of 40 mmHg at FiO 2 of 0.55. Weaning from the ventilator was carried out in a gradual manner with serial improvement in ABG report and marked improvement in serial chest X-rays [Figure 2]. Bilirubin level also corrected to normal level and patient was successfully extubated after 6 days of ventilation.
The present case was very challenging as it posed a huge diagnostic dilemma in accurate diagnosis of malaria as well as the rare respiratory complication in the form of ARDS associated with P. vivax organism. The precise diagnosis was very essential to start an appropriate therapeutic regimen to treat the complicated malaria. The presence of trophozoites and schizonts of P. vivax on peripheral blood smear established the presence of malaria. The negative PfHRP2 immunochromatic assay for P. falciparum further excluded the possibilities of a mixed infection with vivax and falciparum. Moreover, the absence of any other underlying systemic disease including cardiovascular system established the diagnosis of ARDS due to P. vivax malaria. Furthermore, one-step malaria pf/pv rapid test was done to discriminate between P. falciparum and P. vivax, which has 98.2% sensitivity and 99.5% specificity for detecting falciparum infection. Repeated and meticulous examination of peripheral blood film was also carried out to confirm the presence of P. vivax infection. Diagnosis of ARDS was established on the basis of acute onset of respiratory failure with bilateral chest infiltrates on radiograph and PaO 2 /FiO 2 ratio being less than 200, which was 87 in the present case. Normal echocardiography findings excluded the diagnosis of cardiogenic pulmonary edema, which further helped in strengthening our diagnosis. However, the etiopathogenesis leading to pulmonary tissue damage as a result of P. vivax is poorly understood. The invasion of normal red blood cells (RBC) by P. vivax organism does not lead to major pathological changes, which can become decisive in cytoadherence of infested RBCs to endothelial tissues. As a result, the possibilities of microvascular sequestration are far less in vivax infection as compared with falciparum malaria. Most probably, the etiopathogenesis of ARDS in benign malaria is also determined by some other factors. It is also postulated that pulmonary damage leading to altered ventilation perfusion can occur due to monocyte aggregation in lung tissue. These changes are not limited to falciparum alone but can be seen in infection with ovale and vivax species as well. [3] Besides the basic underlying pathology in ARDS being the widespread inflammatory systemic response, it is invariably associated with activation of various inflammatory mechanisms including activation of neutrophils and cytokines. The frequent onset of ARDS after initiation of antimalarial treatment may reflect a posttreatment exacerbation of inflammatory response mediated by proinflammatory cytokine release. The inflammation caused as a result due to such infection raises the possibility of treating such complications with steroids but definite benefits of such therapeutic interventions are lacking. Thus, we used steroids only through inhalational route rather than systemic administration. [1] Recent literary evidence has also confirmed that the adherence of vivax-infested RBCs to endothelial cells occurs through chondroitin sulfate A ligand. The affinity for such adherence is invariably higher in lung, placenta, and tissues of central nervous system. This possibly explains the rare complications of vivax malaria leading to pulmonary injury in the form of acute lung injury (ALI)/ARDS and nervous system involvement. [4],[5],[6] From the clinical evidence of the present case and the published reports, one can draw the inference that vivax is not only associated with uncomplicated malaria alone but can also cause pulmonary and nervous system complications in rare cases. [7] The literary evidence suggests that the widespread use of chloroquine and doxycycline in malaria-endemic areas could be attenuating or diminishing the number of severe cases because of the anti-inflammatory properties of these drugs. However, immune-compromised individuals or those suffering from debilitating diseases may exhibit higher susceptibility to severe complications of P. vivax malaria. [3] Hypoglycemia is the most important complication of quinine for which periodic blood sugar monitoring was carried out in the present case. The most dangerous side effect of quinine especially when being administered i.v. is the occurrence of arrhythmias-in particular ventricular tachycardia. ECG monitoring is therefore very essential, which in the present case did not pose much problem by virtue of the patient being in ICU. High blood concentrations of quinine can cause deafness, blindness, and central nervous sytem (CNS) depression, but these features are very rare. In the present case, besides quinine, no other antimalarial drug was used. Generally, the therapeutic intervention for ARDS involves mechanical ventilation and the same holds true for complicated malaria involving pulmonary parenchyma as was the scenario in the present case. The role of PEEP and titration of oxygen supplementation are very essential for the established case of ARDS in order to prevent any hypoxemic and hyperoxic injury. The role of noninvasive ventilation in management of ALI/ARDS is controversial and that too in infection with vivax malaria. But few reports do claim a good outcome with use of noninvasive ventilation in vivax malaria with involvement of respiratory system resulting in ALI/ARDS. [6] However, studies have supported the definite superior role of invasive ventilation in ALI/ARDS due to malarial infection. [8] However, in the present case, due to respiratory failure and low PaO 2 /FiO 2 ratio, patient had to be managed with invasive ventilation. It was a timely accurate diagnosis and the early administration of antimalarial medication led to a successful outcome. From the present scenario, it can be concluded that early institution of mechanical ventilation with high PEEP in similar cases along with antimalarial administration can prove lifesaving.
Source of Support: Only departmental support, Conflict of Interest: None
[Figure 1], [Figure 2] |
|||||||||||||||||||||||||||||||||||||||||